Utrecht Center for Quantitative Immunology
Why care about quantitative immunology?
Quantifications help us to understand how the immune system works. For instance, the relatively short life span of memory T cells [1] tells us that life long immunity is maintained dynamically, and is not simply stored in long-lived cells. This better understanding moves the field forward because we now need to investigate how the immune system manages to dynamically remember many different memories without them replacing each other. Another example of the impact of finding that memory T cells are short lived comes from the field of HIV-1 infection, where virologists have conveniently assumed that HIV-1 can hide for years in latently infected long-lived memory T cells. Knowing that memory T cells are short-lived calls for novel explanations for the long-term survival of HIV-1 during treatment.We quantified differences between mice in men in how these species maintain their naive T cell pools. Although mice are typically used for studying the effect of aging on the immune system we found that in mice naive T cells are largely produced by the thymus, whereas in human adults naive cells are maintained largely by infrequent divisions, i.e., once every several years [2]. Thus mice are a poor model for studying human aging of naive T cells and their repertoires.
The bioinformatic methods that we develop to identify T cell epitopes allow immunologists and clinicians to scan for the presence of potentially immunogenic epitopes in any pathogen or protein of interest. This provides a more rational approach to vaccine development and immunotherapy. We have recently shown that these methods can be used to screen for neo-antigens in cancer exome data [3]. Individual tumor antigens are essential for the development of personalized cancer immunotherapies. In the context of transplantation these methods can be used to optimize the selection of HLA-mismatched donors, which may lead to survival probabilities similar to HLA-matched donors [4].
It is well established volunteers and animals that are successfully vaccinated against HIV-1 are nevertheless not protected against a normal challenge with this virus. By mathematical modeling we have shown that this can perfectly be understood from that fact that a cytotoxic T cell (CTL) immune response expands slower than the virus replicates [5]. Hence it is crucial to have a sufficiently large memory CTL population at the tissues at which the virus enters, to contain the virus before it starts to replicate faster than the immune response. We study the long-term persistence of memory CTL in local tissues [6], and we study how many infected cells CTL can clear per day [7] to have a better estimate of how many memory CTL need to be maintained in the tissues to provide sterilizing immunity.
Infections with HIV-1 are lethal because naive and memory CD4+ T cell populations get depleted over the years of this chronic infection. Although it is poorly understood how these cells are depleted, a major hypothesis is that HIV-1 infection leads to aberrant activation of the immune system [8]. Using deuterium labeling we quantify the differences in the turnover of naive and memory T cells between healthy volunteers and HIV-1 infected patients in order to better appreciate how immune activation results in depletion of CD4+ T cells.
References
- Sparse production but preferential incorporation of recently produced naive T cells in the human peripheral pool. Vrisekoop N, den Braber I, de Boer AB, Ruiter AF, Ackermans MT, van der Crabben SN, Schrijver EH, Spierenburg G, Sauerwein HP, Hazenberg MD, de Boer RJ, Miedema F, Borghans JA, Tesselaar K. Proc Natl Acad Sci U S A. 2008 Apr 22;105(16):6115-20. doi: 10.1073/pnas.0709713105.
- Maintenance of peripheral naive T cells is sustained by thymus output in mice but not humans. den Braber I, Mugwagwa T, Vrisekoop N, Westera L, Mögling R, de Boer AB, Willems N, Schrijver EH, Spierenburg G, Gaiser K, Mul E, Otto SA, Ruiter AF, Ackermans MT, Miedema F, Borghans JA, de Boer RJ, Tesselaar K. Immunity. 2012 Feb 24;36(2):288-97. doi: 10.1016/j.immuni.2012.02.006.
- Tumor exome analysis reveals neoantigen-specific T-cell reactivity in an ipilimumab-responsive melanoma. van Rooij N, van Buuren MM, Philips D, Velds A, Toebes M, Heemskerk B, van Dijk LJ, Behjati S, Hilkmann H, El Atmioui D, Nieuwland M, Stratton MR, Kerkhoven RM, Kesmir C, Haanen JB, Kvistborg P, Schumacher TN. J Clin Oncol. 2013;31(32):e439-42. doi: 10.1200/JCO.2012.47.7521.
- Predicted indirectly recognizable HLA epitopes presented by HLA-DR correlate with the de novo development of donor-specific HLA IgG antibodies after kidney transplantation. Otten HG, Calis JJ, Kesmir C, van Zuilen AD, Spierings E. Hum Immunol. 2013;74(3):290-6. doi: 10.1016/j.humimm.2012.12.004.
- Understanding the failure of CD8+ T-cell vaccination against simian/human immunodeficiency virus. De Boer RJ. J Virol. 2007 Mar;81(6):2838-48
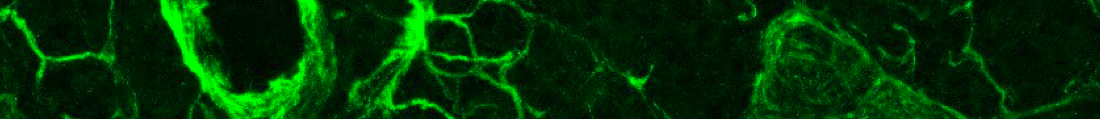
- Tissue-resident memory CD8+ T cells continuously patrol skin epithelia to quickly recognize local antigen. Ariotti S, Beltman JB, Chodaczek G, Hoekstra ME, van Beek AE, Gomez-Eerland R, Ritsma L, van Rheenen J, Maree AF, Zal T, de Boer RJ, Haanen JB, Schumacher TN. Proc Natl Acad Sci U S A. 2012 Nov 27;109(48):19739-44. doi: 10.1073/pnas.1208927109.
- Gadhamsetty S, Beltman JB, Maree AF, de Boer RJ. Biophysical Journal. in press. Killing of targets by CD8 T cells in the mouse spleen follows the law of mass action. Ganusov VV, Barber DL, De Boer RJ. PLoS One. 2011 Jan 24;6(1):e15959. doi: 10.1371/journal.pone.0015959.
- Immune Activation and Collateral Damage in AIDS Pathogenesis. Miedema F, Hazenberg MD, Tesselaar K, van Baarle D, de Boer RJ, Borghans JA. Front Immunol. 2013 Sep 26;4:298.
Members
Jose BorghansRob de Boer
Julia Drylewicz
Can Kesmir
Aridaman Pandit
Leila Perie
Kiki Tesselaar
Johannes Textor
Nienke Vrisekoop
Research
Epitope identificationLymphocyte dynamics
Lymphocyte migration
Relevance
More
UCQI homePhD students
Open positions/projects
Agenda
Publications (pubmed)


